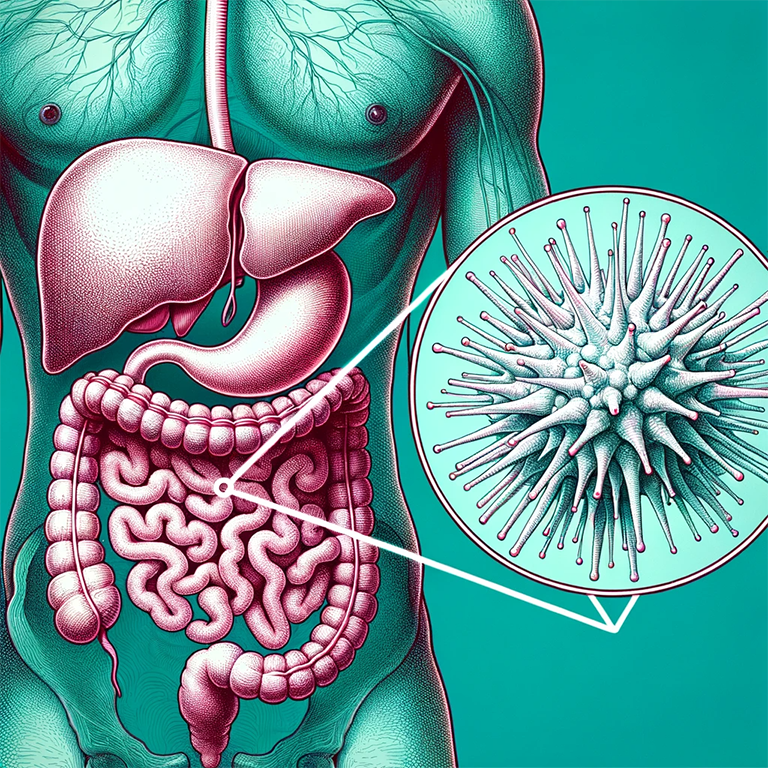
Amoebiasis is a prevalent gastrointestinal infection in humans. Its occurrence is more linked to inadequate sanitation and socio-economic conditions than to specific climatic conditions.
The infection is found globally, with significant health concerns in regions like China, Southeast and West Asia, and Latin America, particularly in Mexico. The ailment results from the parasite Entamoeba histolytica, but only around 10% to 20% of those infected exhibit symptoms. For another tropical disease check the article about Kala-azar/ Leishmaniasis.
Symptoms
The clinical spectrum ranges from asymptomatic infection, diarrhea, and dysentery to fulminant colitis and peritonitis as well as extra-intestinal amoebiasis. Acute amoebiasis can present as diarrhea or dysentery with frequent, small, and often bloody stools.
Chronic amoebiasis can present with gastrointestinal symptoms plus fatigue, weight loss, and occasional fever. Extra-intestinal amoebiasis can occur if the parasite spreads to other organs, most commonly the liver where it causes amoebic liver abscess.
Amoebic liver abscess presents with fever and right upper quadrant abdominal pain. Other organs can also be involved, including pleuropulmonary, cardiac, cerebral, renal, genitourinary, peritoneal, and cutaneous sites.
In developed countries, amebiasis primarily affects migrants from and travelers to endemic regions, men who have sex with men, and immunosuppressed or institutionalized individuals.
Causes
Amoebiasis is caused by the parasite Entamoeba histolytica. Several protozoan species in the genus Entamoeba colonize humans, but not all of them are associated with disease. It exists in two forms- Vegetative (trophozoite) and cystic forms (cyst). Trophozoites multiply and encyst in the colon.
The cysts are excreted in stool and are infective to humans. Cysts remain viable and infective for several days in feces, water, sewage, and soil in the presence of moisture and low temperature.
Transmission occurs via:
- Fecal–oral route, either directly by person-to-person contact or indirectly by eating or drinking faecally contaminated food or water.
- Sexual transmission by oral-rectal contact is also recognized especially among male homosexuals.
- Vectors such as flies, cockroaches, and rodents can also transmit the infection.
The incubation period for E histolytica infection is commonly 2-4 weeks but may range from a few days to years.
The use of night soil for agricultural purposes favors the spread of the disease. Epidemic/outbreaks (occurrence of more cases of a disease than would be expected in a community or region during a given time period) are usually associated with sewage seepage into the water supply.
Diagnosis

Entamoeba histolytica must be differentiated from other intestinal protozoa. Microscopic identification of cysts and trophozoites in the stool is the common method for diagnosing E. histolytica.
Differentiation is based on morphologic characteristics of the cysts and trophozoites. In addition, E. histolytica trophozoites can also be identified in aspirates or biopsy samples obtained during colonoscopy or surgery.
Immunodiagnosis – Antibody Detection
a) Enzyme immunoassay (EIA) is most useful in patients with extra-intestinal disease (i.e., amoebic liver abscess) when organisms are not generally found on stool examination.
b) Indirect hemagglutination (IHA).
If antibodies are not detectable in patients with an acute presentation of suspected amoebic liver abscess, a second specimen should be drawn 7-10 days later. If the second specimen does not show seroconversion, other tests should be considered.
Detectable E. histolytica-specific antibodies may persist for years after successful treatment, so the presence of antibodies does not necessarily indicate acute or current infection.
Antigen Detection
Antigen detection may be useful as an adjunct to microscopic diagnosis in detecting parasites and distinguishing between pathogenic and nonpathogenic infections.
Molecular Diagnosis
Conventional Polymerase chain reaction (PCR)-In reference diagnosis laboratories, molecular analysis by PCR-based assays is the method of choice for discriminating between the pathogenic species (E. histolytica) and the nonpathogenic species (E. dispar).
Radiography, Ultrasonography, Computed tomography (CT), and Magnetic resonance imaging (MRI) can be used for the detection of liver abscesses, and cerebral amoebiasis. Rectosigmoidoscopy and colonoscopy can provide diagnostic information for intestinal amoebiasis.
Management
For symptomatic intestinal infection and extra intestinal disease, treatment with antiamoebic drugs should be taken with consultation of a physician. Asymptomatic patients infected with E. histolytica should also be treated with antiamoebic drugs, because they can infect others and because 4%–10% develop disease within a year if left untreated.
Liver aspiration – Liver aspiration is indicated only if abscesses are large (> 12 cm), abscess rupture is imminent, medical therapy has failed, or abscesses are present in the left lobe.
Complications
Complications of amoebic colitis include the following:
- Fulminant or necrotizing colitis
- Toxic megacolon
- Amoeboma
- Recto vaginal fistula
Complications of amoebic liver abscess include the following:
- Intraperitoneal, intrathoracic, or intrapericardial rupture, with or without secondary bacterial infection
- Direct extension to pleura or pericardium
- Dissemination and formation of brain abscess
Other complications due to amoebiasis include the following:
- Bowel perforation
- Gastrointestinal bleeding
- Stricture formation
- Intussusception
- Peritonitis
- Empyema
Prevention
Amoebiasis can be prevented and controlled both by non-specific and specific measures.
Non-specific measures
- Improved water supply: The cysts are not killed by chlorine in the amount used for water disinfection. Water filtration and boiling are more effective than chemical treatment of water against amoebiasis.
- Sanitation: Safe disposal of human excreta coupled with the sanitary practice of washing hands after defecation and always before handling and consuming food.
- Food safety: Uncooked fruits and vegetables should be washed thoroughly with safe water, peeled fruits, and boiled vegetables prior to eating. Measures should also include the protection of food and drink from flies and cockroaches and the control of these insects. Carriers, who pass cysts and are involved in handling food, whether at home, at street stalls, or in catering establishments, should be actively detected and treated since they are major transmitters of amoebiasis.
- Health education: Elementary hygienic practices, should be propagated and constantly reinforced in schools, health care units, and the home through periodic campaigns using the mass media.
- General social and economic development: Implementation of individual and community preventive measures (e.g., washing of hands, proper excreta disposal) should be an essential part of these activities.
Specific measures
- Community surveys to monitor the local epidemiological situation with regard to amoebiasis.
- Improvement of case management, i.e., rapid diagnosis and adequate treatment of patients with invasive amoebiasis at all levels of health services, including the community and health center levels.
- Surveillance and control of situations that may encourage the further spread of amoebiasis, e.g., refugee camps, and contaminated public water sources.
FAQ
What is the primary mode of transmission of amoebiasis?
The primary mode of transmission is the fecal-oral route, either directly through person-to-person contact or indirectly by consuming contaminated food or water.
Are there any vaccines available for amoebiasis?
As of now, there is no vaccine available for the prevention of amoebiasis.
How long can the cysts of the parasite survive outside the human body?
The cysts can remain viable and infectious for several days in feces, water, sewage, and soil, especially in moist conditions and low temperatures.
Are there any natural remedies?
While there are traditional remedies that some people use, it’s essential to consult a physician for proper diagnosis and treatment.
How can travelers prevent
Travelers should avoid consuming uncooked vegetables, fruits that can’t be peeled, and untreated water. Drinking bottled or boiled water can reduce the risk.
Final Words
Amoebiasis, a global health concern, underscores the importance of sanitation, clean water, and proper hygiene practices. While treatments are available, prevention remains the most effective strategy against this gastrointestinal infection.
Awareness, education, and infrastructure development are crucial in combating the spread of this disease.