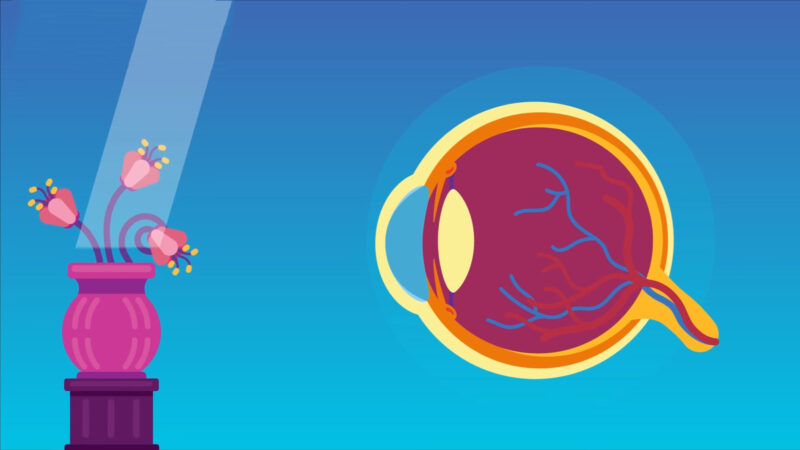
Hypermetropia (hyperopia, long-sightedness or far- sightedness) is a form of refractive error in which parallel rays of light coming from infinity are focused behind the light sensitive layer of the retina, when the eye is at rest.
Donders (1864) discusses in his historical review about hypermetropia. Much of the problem was caused by confusion between the effects of presbyopia and hypermetropia on near vision.
Small hypermetropia may be corrected by voluntary accommodation. Even high errors of refraction may be corrected this way, but convex glasses may be required if symptoms are not relieved.
Emmetropia is the condition where the eye has no refractive error and requires no correction for distance vision. Refractive error (ametropia) results when cornea and lens inadequately focus the light rays, resulting in blurred images. The measuring unit for refractive error is dioptre (D), which is defined as the reciprocal of the focal length in meters.
In hypermetropia, the cornea is flatter or the axial length is too short. Therefore, the images do not focus by the time they reach to the retina. For clear vision, a hypermetropic eye must accommodate to increase its lenticular power to bring distant objects in focus on retina. This requires contraction of ciliary muscle, and therefore, far-sighted eye is never at rest and work even harder to see near objects clearly. Hypermetropic corrections add positive focusing power to the eye for clear vision.
Accommodation: The degree of hypermetropia corrected by accommodative effort is known as facultative hypermetropia. Remaining uncorrected hypermetropia is called absolute hypermetropia. Total hypermetropia after abolishing voluntary accommodation is known as manifest hypermetropia (facultative plus absolute). With advancing age, accommodative effort cannot be sustained, and hypermetropia becomes absolute till the effort of accommodation fails to correct any hypermetropia. Thus the facultative hypermetropia becomes abolished and there remains no difference between absolute and manifest hypermetropia.
Some of the hypermetropia is corrected by the inherent tone of the ciliary muscles and this is called latent hypermetropia. The degree of latent hypermetropia is high in young persons and becomes less with advancing age. Complete cycloplegia (paralysis of accommodation) can abolish latent hypermetropia. The refractive error estimated under complete cycloplegia is called total hypermetropia (manifest plus latent).
Symptoms
The symptoms vary depending upon the age of the patient and the severity of refractive error. Patient may be asymptomatic. Small amount of refractive error in young patients is usually corrected by mild accommodative effort, without producing any symptoms.
Symptomatic patients may present with:
When hypermetropia is fully corrected: At times the hypermetropia is fully corrected (thus vision is normal) but due to sustained accommodative efforts the patient develops asthenopic symptoms.
- Asthenopia (eyestrain).
- Frontal or fronto-temporal headache.
- Watering.
- Mild aversion to light.
These symptoms worsen as the day progresses and are aggravated by prolonged near work.
When hypermetropia is not fully corrected: When hypermetropia is not fully corrected by the voluntary accommodative efforts, then the patient complains of defective vision more for near than distance, due to sustained accommodative effort. Patient present with:
- Asthenopia.
- Defective vision more for near.
When hypermetropia is high: When hypermetropia is high (more than 4 D), the patients usually do not accommodate and they suffer with:
- Marked defective vision for both near and distance.
When there is more of absolute hypermetropia: With ageing the eye move from latent and facultative hypermetropia to greater degrees of absolute hypermetropia. This leads to progressive defective vision. Patient present with:
- Blurring of vision at a younger age than in emmetrope.
When there is Spasm of accommodation: Spasm of accommodation may induce pseudo-myopia. It may be detected by cycloplegic refraction. It presents as:
- Intermittent sudden blurring of vision.
In general, child may also present with lid diseases (like blepharitis, stye or chalazion), convergent squint or amblyopia.
Causes
Hypermetropia may be:
- Axial hypermetropia: Axial hypermetropia is the commonest type. The total refractive power of the eye is normal but there is axial shortening of the eyeball. About 1 mm shortening of the antero-posterior length of the eye results in about 3 Dioptres (D) of hypermetropia.
- Curvature hypermetropia: Curvature hypermetropia is that condition in which curvature of the cornea, lens or both is increased (flatter) than the normal, resulting in change in refractive power of the eye. About 1 mm increase in radius of curvature results in 6 D of hypermetropia.
- Index Hypermetropia: Index Hypermetropia occurs due to change in refractive index of the crystalline lens with age.
- Positional hypermetropia: Positional hypermetropia results from posteriorly placed crystalline lens of the eye.
- Absence of crystalline lens: Absence of crystalline lens either congenital absence or acquired (following surgical removal or posterior displacement) leads to aphakia. There is high hypermetropia in aphakia.
It may also be functional, as is seen in presbyopia or may be induced by cycloplegic drugs.
Diagnosis
Diagnosis of hypermetropia is based on the symptoms and clinical signs observed.
Clinical signs:
- Visual acuity: Visual acuity varies with degree of hypermetropia and power of accommodation. Patients with low degree of refractive error may have normal visual acuity. However, there is decrease in visual acuity for seeing near objects.
- Cover test: Cover test reveals an accommodative convergent squint. Due to altered accommodative convergence (AC) and accommodation (A) balance (AC/A ratio), maintaining binocular vision becomes difficult. The advantages of binocular vision are sacrificed in favour of more obvious advantages of clear vision. The better eye dominates for vision and the other eye develops accommodative convergent squint.
- Eyelids: One may develop blepharitis, stye or chalazion. The correlation between lid conditions and hypermetropia is not clear.
- Eyeball: Size of the eyeball may be normal or small.
- Cornea: Cornea may also be slightly smaller in size. There may be associated condition of cornea plana (flat cornea).
- Anterior chamber: Anterior chamber is relatively shallow in high hypermetropia.
- Glaucoma: The eye is small in high hypermetropia along with small size of cornea and shallow anterior chamber. Due to increase in size of the lens with ageing, the eye becomes prone to an attack of narrow angle closure glaucoma.
- Lens: Lens may be dislocated backwards.
- Fundus: Fundus examination shows small optic disc which may look hyperaemic (vascular) with ill- defined margins. This appearance may simulate papillitis. Since there is no swelling of the disc, it is called pseudo-papillitis. The retina is shiny due to reflection of light, called as shot silk appearance. Reflex of retinal vessels may be accentuated simulating arteriosclerotic changes. Vessels may be tortuous and may show abnormal branching.
- Ultrasonography or biometry: A- scan ultrasonography or biometry may show decreased antero- posterior length of the eyeball.
Severity of hypermetropia:
Based on severity, hypermetropia may be classified as:
- Low: Up to + 2 D.
- Moderate: From + 2.25 to 5 D.
- High: More than + 5 D, and rarely it exceeds 6 – 7 D, which is equivalent to 2 mm shortening of the optic axis. Individual cases of much higher degrees (e.g. up to 24 D), without any other associated anomaly have been recorded.
Clinical types of hypermetropia:
I. Simple hypermetropia: Simple hypermetropia is the commonest type. It includes axial and curvature hypermetropia due to biological variations in the development of the eye. It may be hereditary.
II. Pathological hypermetropia: Pathological type is due to congenital or acquired conditions outside the normal biological variation of development. It may be
- Senile or acquired hypermetropia: It occurs in old age due to
– Curvature hypermetropia: There is decreased curvature of the outer lens fibres with ageing.
– Index hypermetropia: It is due to acquired sclerosis of the cortex (outer part) of crystalline lens. In young age, refraction of the cortex is less than nucleus (central part) of the lens. This inequality results in formation of a central lens surrounded by two converging menisci. This increases the refracting power of the lens. With ageing, this differentiation diminishes and the lens becomes more homogeneous with reduced converging power.
- Positional hypermetropia: It may occur due to posterior subluxation (partial dislocation) of the lens.
- Aphakic hypermetropia: Aphakia is the displacement of the lens from its normal pupillary position in the eye. It may be congenital or acquired condition. The eye is hypermetropic with marked defective vision for near and distance. On an average there is need of + 10 or + 11 D lens for correction.
- Consecutive hypermetropia: It is due to surgically overcorrected myopia or pseudo-phakia (eye with intraocular lens following removal of crystalline lens as in cataract surgery) with under-correction.
III. Functional hypermetropia: It results from paralysis of accommodation as is seen in patients with third intracranial nerve palsy and internal ophthalmoplegia.
Management
Medical optical therapy:
Assessment of Vision:
The most common component of assessment of visual function is to test central vision through visual acuity. Visual acuity determines ability to read symbols of varying sizes at a standard testing distance. This reference distance approximates optical infinity and is typically 6 meters. A 6/6 letter on the standard eye chart devised by Snellen is considered normal visual acuity. Refractive errors may result in uncorrected visual acuities that fall below 6/6. In the absence of other diseases, the condition of hypermetropia may be corrected with restoration of normal visual function. This may be achieved with spectacles or contact lenses.
Basic principle of therapy is to converge and focus the light rays on the retina with the help of convex (plus) glasses.
Rules for prescribing glasses in hypermetropia:
- Cycloplegia: Total hypermetropia is determined by performing refraction (checking power of glasses) under complete cycloplegia.
- Small total manifest hypermetropia: For small total manifest hypermetropia e.g. 1 D or less, correction may be required only if the patient is symptomatic.
- Spherical power: Spherical power is prescribed to the extent that it is suitably acceptable to the patient.
- Astigmatism: Astigmatism should be fully corrected.
- Children younger than 4 years: Children younger than 4 years requiring hypermetropic correction may usually accept full cycloplegic correction. It may be reduced in older children.
- Older children: Older children may not accept full cycloplegic correction because of the blur for distance. It may be increased gradually till the child accepts for the manifest hypermetropia.
- Exophoria: Hypermetropia should be under-corrected by about 1- 2 D if there is associated exophoria.
- Accommodative convergent squint: Full cycloplegic correction should be given if there is accommodative convergent squint.
- Amblyopia (lazy eye): In the presence of associated amblyopia (Functionally reduced vision not correctable with glasses and is not due to any eye disease) in one eye, full correction with occlusion therapy should be given.
- Growth of child: Hypermetropia decreases with growth of the child. Periodic refraction should be conducted and the correction should be reduced accordingly.
Prescription of convex power:
- Spectacles: Convex lenses may be prescribed as spectacles.
- Contact lenses: Contact lenses may be prescribed for cosmetic reasons once the refractive power of the eye stabilises. Contact lenses may be prescribed for unilateral hypermetropia as well.
Surgical therapy:
It may be
- Non- contact Holmium:YAG laser thermokeratoplasty: Non- contact Holmium:YAG laser thermokeratoplasty is suitable for hypermetropia of about + 1 D to + 2.5 D. With this, multiple radially distributed spots are produced in the para-central cornea, which leads to shrinkage of the collagen in the mid- peripheral stroma and consequent steepening of the central cornea.
- Hypermetropic photorefractive keratectomy (H- PRK): The principle of this procedure is to steepen the anterior corneal curvature. The cornea is sculpted in to a steeper convex lens by creating a furrow- like ring zone in the corneal periphery.
- Conductive keratoplasty: Conductive keratoplasty is a non-invasive procedure in which radiofrequency is used to correct low hypermetropia with or without astigmatism. It may also be used to correct residual refractive error after cataract surgery or laser assisted in- situ keratomileusis.
- Hypermetropic laser assisted in- situ keratomileusis (LASIK): It is used to correct mild- to- moderate hypermetropia varying from + 1 D to + 4 D.
- Phakic intraocular lens (IOL) implants: Phakic intraocular lens (IOL) implants are used to correct higher degrees of hypermetropia, varying from about + 4 D to + 10 D. Phakic IOLs are especially designed, foldable, convex, thin lenses implanted in the posterior chamber behind the iris and in front of the normal crystalline lens.
- Refractive lens exchange: Extraction of clear lens with implantation of an IOL, preferably foldable IOL or a piggyback IOL. In piggyback IOL, two IOLs are placed in the eye one on top of the other. This is done if the biometry is + 40 D or so, and one does not have a lens of high power to implant. Moreover, there is high level of spherical aberration with thick lenses.
Prognosis:
Asymptomatic children up to about 10 years with low to moderate hypermetropia usually do not require any glasses. Visual acuity decreases as the child grows due to loss of accommodation.
Hypermetropia decreases quality of life. Poor vision may also decrease in the ability to learn and develop. Hypermetropia that is not fully compensated with accommodation may produce complications.
Complications
Uncorrected hypermetropia may produce complications such as:
- Accommodative convergent squint: Excessive use of accommodation may produce accommodative convergent squint, usually by the age of about 2- 3 years.
- Amblyopia: Amblyopia may develop as
– Anisometropic amblyopia as in cases with unequal or unilateral hypermetropia.
– Strabismic amblyopia as in children who develop accommodative squint.
– Ametropic amblyopia as seen in children with uncorrected bilateral high hypermetropia.
- Lid diseases: Repeated rubbing of eyes in hypermetropic blurred vision may produce blepharitis, stye or chalazion.
- Primary narrow angle glaucoma: The eye in hypermetropia is proportionately small. The size of the lens keeps on increasing with age. This predisposes the already small eye to the primary narrow angle glaucoma.
References:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1771184
http://onlinelibrary.wiley.com/doi/10.1111/opo.12168/pdf
http://eyewiki.aao.org/Hyperopia
http://eyewiki.aao.org/Conductive_Keratoplasty