Heterophoria, also known as latent squint, is a condition that affects the alignment of the eyes. While it may sound complex, this article aims to break down the topic into easily digestible sections, providing valuable insights for a diverse readership.
This is a condition where the eyes, in their primary position or movement, are maintained on the fixation point under stress only with the aid of corrective fusion reflexes. When this fusion is removed, one eye’s visual axis deviates.
Definition and History
George T Stevens introduced the term “heterophoria” in 1886. He described it as an abnormal adjustment of the eye muscles, which applies to strabismus as well.
In heterophoria, binocular vision is maintained, but it requires more force than in the perfect equilibrium of the ocular muscles. This deviation is kept latent by the fusion mechanism. The term “heterophoria” is derived from the Greek words “heteros,” meaning different, and “phoria,” meaning bringing.
Orthophoria vs. Heterophoria
Orthophoria is characterized by the perfect alignment of both eyes in all positions, making the visual axes parallel for distance and proper convergence for near. However, true orthophoria is rare. Most individuals have a small amount of heterophoria present.
Symptoms

Heterophoria can be divided into two types based on symptoms: compensated and de-compensated.
Compensated
Compensated heterophoria is not associated with any symptoms. The compensation depends on the reserve neuromuscular power to overcome the muscular imbalance.
De-compensated Heterophoria
When the fusion amplitudes are inadequate to control deviation, symptoms arise. These include:
- Muscular fatigue symptoms:
- Headache
- Asthenopia (eyestrain)
- Photophobia (sensitivity to light)
- Difficulty in changing focus from near to distance and vice versa.
- Binocular single vision (BSV) failure symptoms:
- Blurred vision
- Crowding of words while reading
- Difficulty with stereopsis
- Intermittent diplopia
- Intermittent squint without diplopia.
- Postural sensation defects:
- Problems in judging distances and positions, especially of moving objects.
Causes
The causes of heterophoria can be grouped into several categories.
Static Causes (Anatomical Factors)
These include:
- Orbital asymmetry
- Interpupillary distance abnormalities
- Size and shape of the eyes
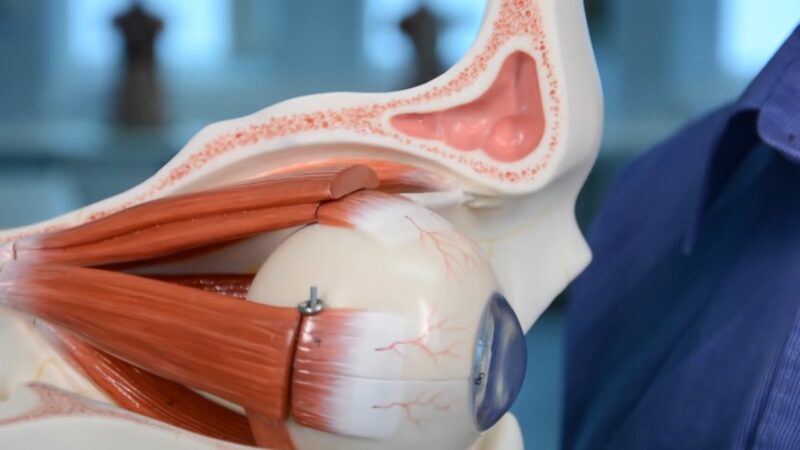
- Abnormal strength or structure of extra-ocular muscles
- Volume of retro-bulbar tissue and orbital fascias
- Anomalous central distribution of the tonic innervations of eyes
- Variation in the optical axis of the eye.
Kinetic Causes (Physiological Factors)
Factors include:
- Age-related tendencies towards esophoria or exophoria
- Convergence and accommodation changes
- Dissociation factors, such as prolonged use of one eye.
Neurogenic Causes
Lower motor neuron diseases lead to incomitant heterophoria, while upper motor neuron diseases result in comitant heterophoria.
Risk Factors for De-compensated Heterophoria
These include:
- General debility and lowered vitality
- Mental stress
- Inadequate fusion reserve
- Advancing age
- Precision jobs.
Sensorial adaptations, such as abnormal retinal correspondence and image suppression, may develop to avoid foveal diplopia. Intermittent heterotropia is when heterophoria breaks into heterotropia, causing the patient to sometimes experience heterophoria and sometimes heterotropia.
Diagnosis

Diagnosing involves various methods, and it’s essential to understand that heterophorias can be as significant as heterotropias.
Examination and History
A detailed history and determination of refractive error are crucial. Ocular movements should also be tested in all gaze positions.
Cover-Uncover Test
This test is performed for both distance and near vision. It involves covering one eye while the other fixates on a distant target. Any movement of the eye when uncovered is noted.
Alternate Cover Test
This test induces dissociation to reveal total deviation when fusion is disrupted.
Maddox Rod Test
The Maddox rod consists of fused cylindrical red glass rods that convert a white light spot into a red streak. This test helps determine the degree and direction of deviation.
Maddox Wing Test
This test measures the degree of heterophoria at near fixation.
Synoptophore
This device can also measure the degree.
Near Point Tests
The near point of convergence and the near point of accommodation are crucial measurements in diagnosing heterophoria.
Measurement of Fusion Reserves
Fusion amplitudes measure the efficacy of vergence movements and can be tested with prism bars or the synoptophore.
Clinical Types
These include exophoria, esophoria, hyperphoria, hypophoria, cyclophoria, and anisophoria.
Differential Diagnosis
It’s essential to differentiate heterophoria from heterotropias.
Management

Managing heterophoria is crucial, especially for de-compensated types. While minor heterophoria without symptoms might not require treatment, it’s essential to address significant cases to ensure visual comfort and prevent further complications.
Medical Therapy
I. Optical Management
Esophoria:
- Full correction of hypermetropia (+1.25 dioptres or more) when detected during refraction.
- For patients with a high AC/A ratio and symptomatic esophoria without hypermetropia, miotics or bifocal glasses might be beneficial.
- Base-out prisms can provide visual comfort for those with non-accommodative esophoria.
Exophoria:
- Treatment is not required for patients without asthenopia.
- Addressing significant refractive errors, especially anisometropia, aniseikonia, aphakia, and astigmatism, can produce sharp retinal images, increasing the stimulus to fuse.
- Minus lenses can decrease exodeviation in patients with a high AC/A ratio.
Hyperphoria:
- Prisms in glasses can be tried in selective cases of hyperphoria.
II. Orthoptics:

Orthoptic exercises are the primary treatment for patients with moderate degrees of exophoria or esophoria who have a fair degree of binocular function. These exercises help train the eyes to work together and can be particularly beneficial for those with convergence insufficiency.
III. Miotic Drugs:
Miotic drugs can be useful for near esophoria due to a high AC/A ratio. These drugs facilitate peripheral accommodation, requiring less than normal innervation and consequently less than normal accommodative convergence.
Surgical Therapy
Surgery is considered for patients with intermittent exotropia showing signs of worsening. The aim of the surgical procedure is either to strengthen the weak muscle or to weaken the strong muscle. The decision to undergo surgery should be made after thorough consultation with an ophthalmologist.
FAQ
1. Is heterophoria the same as lazy eye?
No, heterophoria is not the same as lazy eye (amblyopia). While both conditions involve the eyes, amblyopia is a vision development disorder where one eye doesn’t achieve normal visual acuity, even with prescription lenses.
2. Can heterophoria be cured?
While heterophoria can’t be “cured” in the traditional sense, its symptoms can be managed effectively with optical corrections, orthoptic exercises, and in some cases, surgery.
3. Does heterophoria get worse with age?
Heterophoria can change with age, especially if it’s de-compensated. Factors like general debility, mental stress, advancing age, and precision jobs can exacerbate the condition.
4. Can it cause anxiety?
Yes, in some cases, heterophoria can cause anxiety. Many patients struggle with conflicting signals between their eyes and inner ear, leading to feelings of discomfort and anxiety in specific situations.
5. Is it hereditary?
There isn’t conclusive evidence to suggest that heterophoria is hereditary, but some eye conditions can have a genetic component. It’s always a good idea to know your family’s eye health history.
6. Can screen time affect heterophoria?
Excessive screen time can strain the eyes and might exacerbate symptoms in individuals with heterophoria, especially if they are not wearing the correct prescription glasses.
7. How often should someone with heterophoria have eye exams?
Individuals with heterophoria should have regular eye exams, typically once a year, to monitor the condition and ensure that they have the correct optical corrections.
Conclusion
Heterophoria, while not as commonly discussed as other eye conditions, plays a significant role in many individuals’ visual experiences. Understanding its symptoms, causes, and management options is crucial for both patients and healthcare providers.
With the right approach, those affected by it can achieve better visual comfort and overall eye health. Whether through optical adjustments, orthoptic exercises, or surgical interventions, there are multiple avenues to address and manage this condition effectively.

