With the percentage of infertility getting very high, being pregnant is a blessing. If you are lucky enough, making sure you’re informed about any potential complications during a pregnancy is essential.
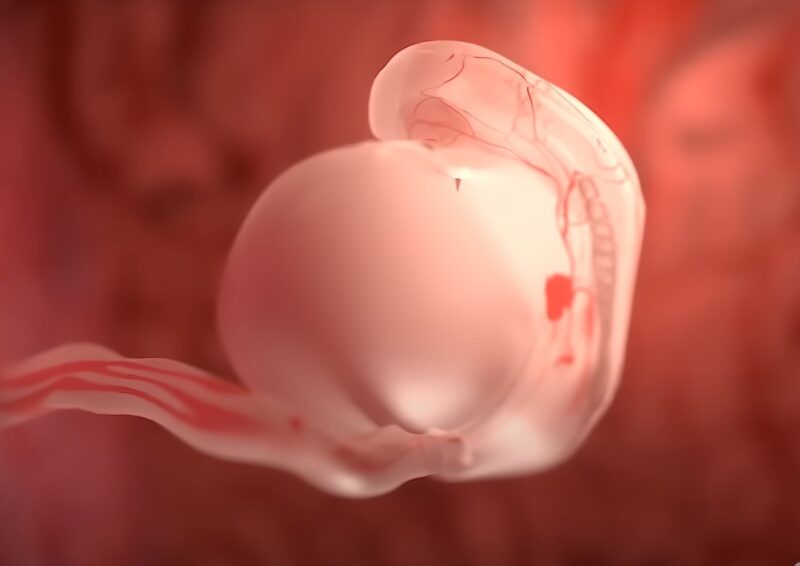
One of these can be Intrauterine Growth Restriction (IUGR). It is a term that might sound complex, but it’s crucial for expecting parents and medical professionals to understand. It’s a condition that affects the unborn baby, making them smaller or less developed than expected for their gestational age. But what causes it? How is it diagnosed and managed? And most importantly, how can it be prevented?
Intrauterine Growth Restriction (IUGR) is a prevalent complication in pregnancies, especially in developing countries. It poses a heightened risk of perinatal mortality and morbidity. Simply put, IUGR refers to a scenario where the fetus is smaller than normal for its gender and gestational age.
IUGR is when the fetal weight is below the 10th percentile for its gestational age, as determined by an ultrasound. If a baby’s birth weight is less than 2,500 g (5lb, 8oz) at term, it’s considered IUGR. This condition is sometimes also referred to as “small for gestational age” or “fetal growth restriction.”
Types

There are two primary classifications of IUGR:
- Symmetric or primary: Here, all internal organs are reduced in size. This type accounts for 20%-30% of all IUGR cases.
- Asymmetric or secondary IUGR: The baby’s head and brain are of regular size, but the abdomen is smaller. This type becomes evident mostly in the 3rd trimester and is more common, found in 70%-80% of IUGR cases.
Causes
IUGR can be attributed to various factors related to the mother, fetus, and placenta.
Maternal Causes
Several maternal factors can contribute to IUGR:
- Before Pregnancy: Factors include low pre-pregnancy weight, poor nutritional status, low socioeconomic status, having more than five births, or a recent pregnancy.
- During Pregnancy: Factors include inadequate weight gain, excessive physical work, chronic illnesses, drug use, smoking, alcohol consumption, hypertension, and decreased oxygen availability.
Uterine and Placental Factors
These include:
- Inadequate placental growth
- Uterine malformations
- Decreased utero-placental blood flow
- Multiple gestations
Fetal Causes
These are primarily due to genetic abnormalities, intrauterine infections, and other conditions. Symmetric IUGR is often due to genetic causes, early gestational infections, and maternal alcohol use. In contrast, asymmetric IUGR is usually due to conditions affecting the fetus later in gestation.
Diagnosing
Accurate diagnosis is crucial for the effective management of IUGR.
Fundal Height Measurement
This is the most straightforward method. After the 20th week of pregnancy, the size of the uterus, measured from the pubic bone to its top, usually corresponds with the pregnancy’s number of weeks. A lag suggests.
Weight Checkups
Regular monitoring of the mother’s weight during prenatal checkups can indicate potential growth problems in the baby.
Ultrasound and Doppler Assessment
Ultrasound measures the baby’s head and abdomen to estimate its weight. Doppler assessment, on the other hand, checks the blood flow in the umbilical cord and the baby’s brain vessels. Abnormal results can diagnose IUGR.
Managing

Addressing IUGR promptly and effectively is crucial for the well-being of both the mother and the baby.
General Management Measures
These encompass treating any maternal diseases, ensuring the mother receives adequate nutrition, and recommending bed rest.
Monitoring and Delivery
For babies showing signs of abnormal function during biophysical profile testing, preterm delivery might be necessary. It’s crucial to administer antenatal steroids in preterm pregnancies and ensure delivery at a facility equipped with emergency obstetric and neonatal care units. Continuous fetal monitoring during labor is essential to minimize fetal hypoxia.
Complications

IUGR can lead to various health challenges during pregnancy, delivery, and post-birth.
During Delivery
Babies with IUGR might face:
- Difficulty during vaginal delivery
- Low Apgar scores, indicating potential health concerns
- Meconium aspiration, leading to respiratory issues
Post-Birth Challenges
Babies diagnosed with experience:
- Low birth weight
- Hypoglycemia or low blood sugar
- Increased red blood cell count
- Reduced resistance to infections
- Difficulty in maintaining body temperature
Prevention
While IUGR can sometimes occur despite a mother’s best efforts, certain measures can reduce its risk.
Pre-Pregnancy Care
Ensuring women receive care both before and between pregnancies can significantly improve outcomes. This includes:
- Adopting a healthy diet and regular physical activity
- Managing chronic diseases like hypertension and diabetes
- Correcting anemia and ensuring folic acid supplementation
Care During Pregnancy
To ensure the best outcomes:
- Only consume medications prescribed by healthcare professionals
- Maintain a balanced diet and consider fortified foods
- Get adequate rest and sleep
- Avoid tobacco, smoking, and alcohol
Delivery Care
It’s recommended to plan the delivery in health facilities equipped with emergency obstetric and neonatal care facilities.
Frequently Asked Questions (FAQs)
1. Can It be detected early in pregnancy?
While some early signs might hint at IUGR, definitive diagnosis usually occurs after the 20th week of pregnancy through fundal height measurements, weight checkups, and ultrasounds.
2. Does IUGR mean my baby will have long-term health issues?
While some babies with IUGR might face challenges like growth retardation and neurodevelopment defects, many grow up without any long-term complications. Regular check-ups and early interventions can help manage potential issues.
3. Can It be cured?
IUGR can’t be “cured” in the traditional sense, but with proper management, many of its effects can be mitigated. This includes monitoring the baby’s growth, ensuring the mother’s health, and sometimes considering early delivery.
4. Are there any lifestyle changes I can make to prevent?
Yes, maintaining a healthy lifestyle before and during pregnancy can reduce the risk. This includes a balanced diet, avoiding tobacco, alcohol, and certain medications, and managing chronic health conditions.
5. Is It the same as being born small?
Not necessarily. While IUGR babies are often small for their gestational age, not all small babies have IUGR. Some babies are naturally small but perfectly healthy.
Final Words
Intrauterine Growth Restriction (IUGR) is a condition that can be concerning for expecting parents. However, with the right knowledge, timely interventions, and a supportive healthcare team, many of the challenges associated with IUGR can be effectively managed. Always prioritize open communication with your healthcare provider and stay informed to ensure the best outcomes for both mother and baby.

